https://www.aafp.org/afp/2014/0201/p180.html
The most common etiology is viral gastroenteritis, a self-limited disease.
Risk factors and signs of inflammatory diarrhea and/or severe dehydration can direct any needed testing and treatment.
Most patients do not require laboratory workup, and routine stool cultures are not recommended.
Treatment focuses on preventing and treating dehydration.
Diagnostic investigation should be reserved for patients with severe dehydration or illness, persistent fever, bloody stool, or immunosuppression, and for cases of suspected nosocomial infection or outbreak.
Oral rehydration therapy with early refeeding is the preferred treatment for dehydration. Antimotility agents should be avoided in patients with bloody diarrhea, but loperamide/simethicone may improve symptoms in patients with watery diarrhea.
Probiotic use may shorten the duration of illness.
When used appropriately, antibiotics are effective in the treatment of shigellosis, campylobacteriosis, Clostridium difficile, traveler's diarrhea, and protozoal infections.
Prevention of acute diarrhea is promoted through adequate hand washing, safe food preparation, access to clean water, and vaccinations.
Acute diarrhea is defined as stool with increased water content, volume, or frequency that lasts less than 14 days.
In patients with acute diarrhea, stool cultures should be reserved for grossly bloody stool, severe dehydration, signs of inflammatory disease, symptoms lasting more than three to seven days, immunosuppression, and suspected nosocomial infections.
Routine testing for ova and parasites in acute diarrhea is not necessary in developed countries, unless the patient is in a high-risk group (i.e., diarrhea lasting more than seven days, especially if associated with infants in day care or travel to mountainous regions; diarrhea in patients with AIDS or men who have sex with men; community waterborne outbreaks; or bloody diarrhea with few fecal leukocytes).
The first step to treating acute diarrhea is rehydration, preferably oral rehydration.
Combination loperamide/simethicone may provide faster and more complete relief of acute nonspecific diarrhea and gas-related discomfort than either medication alone.
Antibiotics (usually a quinolone) reduce the duration and severity of traveler's diarrhea.
Clinically, acute infectious diarrhea is classified into two pathophysiologic syndromes, commonly referred to as noninflammatory (mostly viral, milder disease) and inflammatory (mostly invasive or with toxin-producing bacteria, more severe disease)
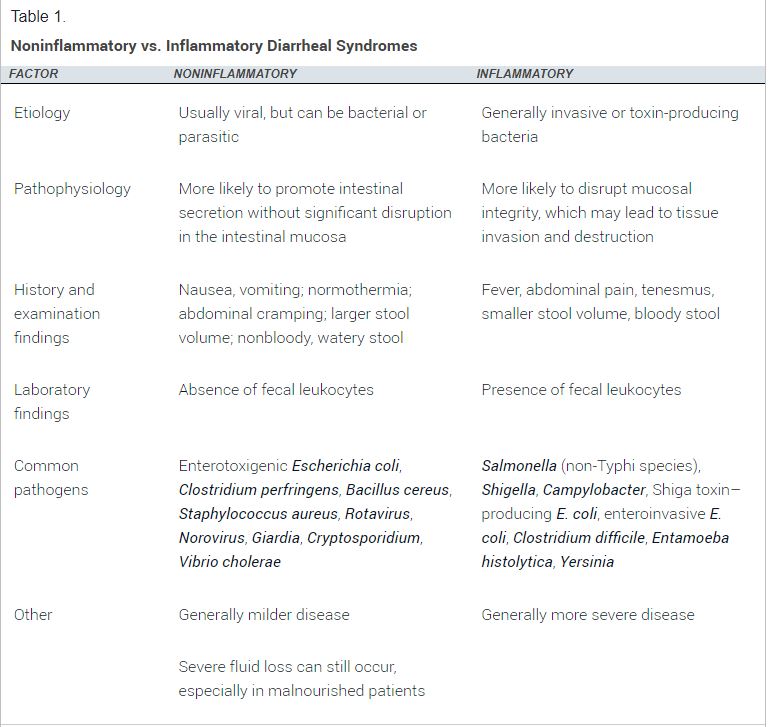
Bacterial infections are more often associated with travel, comorbidities, and foodborne illness
Salmonella, Campylobacter, Shigella, and Shiga toxin–producing Escherichia coli (enterohemorrhagic E. coli).
HISTORY
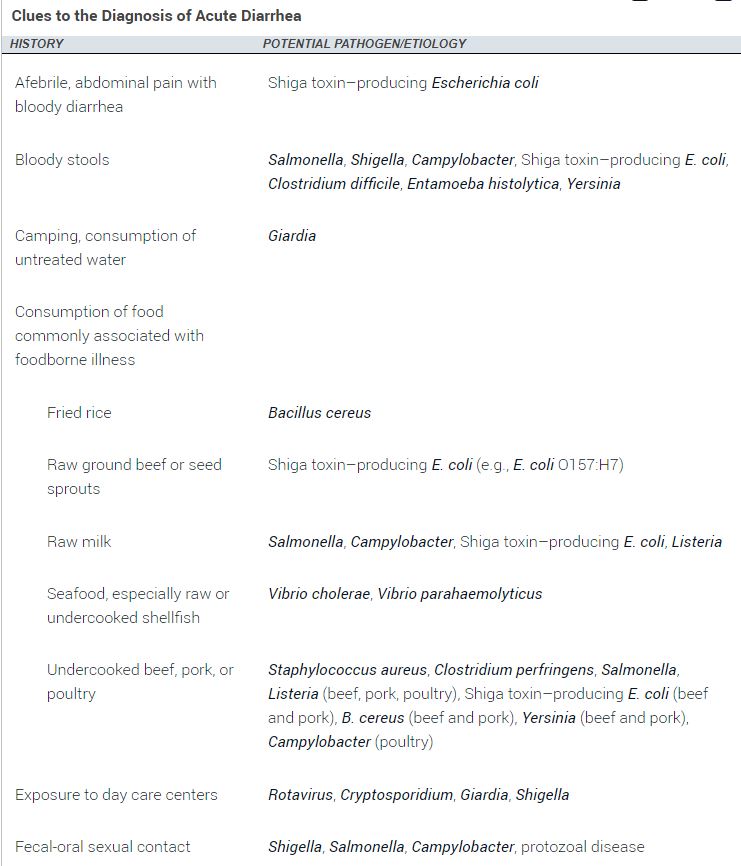
The onset, duration, severity, and frequency of diarrhea should be noted, with particular attention to stool character (e.g., watery, bloody, mucus-filled, purulent, bilious).
evaluated for signs of dehydration, including decreased urine output, thirst, dizziness, and change in mental status
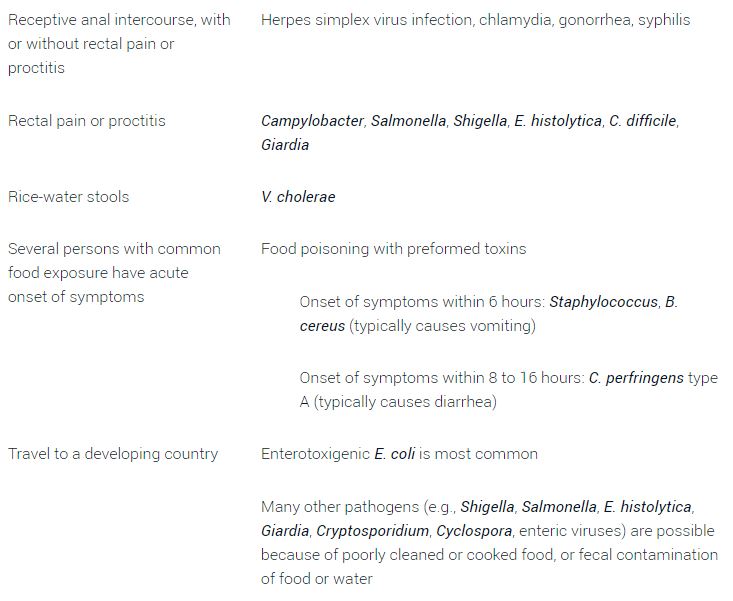
Vomiting is more suggestive of viral illness or illness caused by ingestion of a preformed bacterial toxin.
Symptoms more suggestive of invasive bacterial (inflammatory) diarrhea include fever, tenesmus, and grossly bloody stool.
A food and travel history is helpful to evaluate potential exposures.
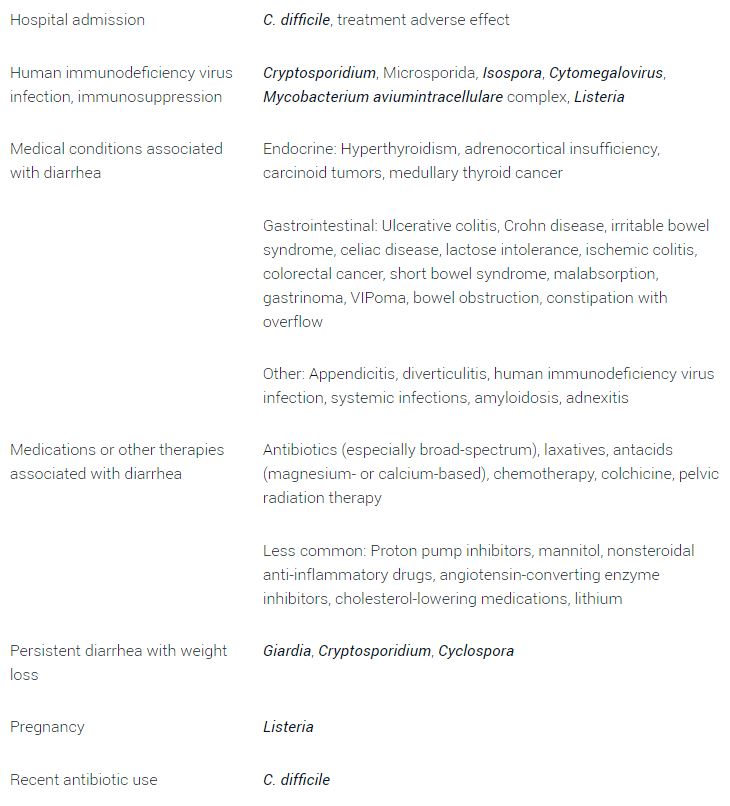
Children in day care, nursing home residents, food handlers, and recently hospitalized patients are at high risk of infectious diarrheal illness. Pregnant women have a 12-fold increased risk of listeriosis, which is primarily contracted by consuming cold meats, soft cheeses, and raw milk.
Recent sick contacts and use of antibiotics and other medications should be noted in patients with acute diarrhea. Sexual practices that include receptive anal and oral-anal contact increase the possibility of direct rectal inoculation and fecal-oral transmission.
The history should also include gastroenterologic disease or surgery; endocrine disease; radiation to the pelvis; and factors that increase the risk of immunosuppression, including human immunodeficiency virus infection, long-term steroid use, chemotherapy, and immunoglobulin A deficiency.
The primary goal of the physical examination is to assess the patient's degree of dehydration. Generally ill appearance, dry mucous membranes, delayed capillary refill time, increased heart rate, and abnormal orthostatic vital signs can be helpful in identifying more severe dehydration. Fever is more suggestive of inflammatory diarrhea.
Diagnostic Testing
OCCULT BLOOD
LEUKOCYTES AND LACTOFERRIN
STOOL CULTURES : grossly bloody stool, severe dehydration, signs of inflammatory disease, symptoms lasting more than three to seven days, or immunosuppression.
CLOSTRIDIUM DIFFICILE TESTING patients who develop unexplained diarrhea while using antibiotics or within three months of discontinuing antibiotics.
OVA AND PARASITES Indications for ova and parasite testing include persistent diarrhea lasting more than seven days, especially if associated with infants in day care or travel to mountainous regions; diarrhea in persons with AIDS or men who have sex with men; community waterborne outbreaks; or bloody diarrhea with few fecal leukocytes
ENDOSCOPY
Treatment

REHYDRATION THERAPY
FEEDING BRAT diet (bananas, rice, applesauce, and toast) and the avoidance of dairy are commonly recommended, supporting data for these interventions are limited
ANTIDIARRHEAL MEDICATIONS loperamide (Imodium) may reduce the duration of diarrhea. loperamide/simethicone combination has demonstrated faster and more complete relief of acute nonspecific diarrhea and gas-related discomfort compared with either medication alone. Loperamide may cause dangerous prolongation of illness in patients with some forms of bloody or inflammatory diarrhea and, therefore, should be restricted to patients with nonbloody stool.
antisecretory drug bismuth subsalicylate (Pepto-Bismol) is a safe alternative in patients with fever and inflammatory diarrhea.
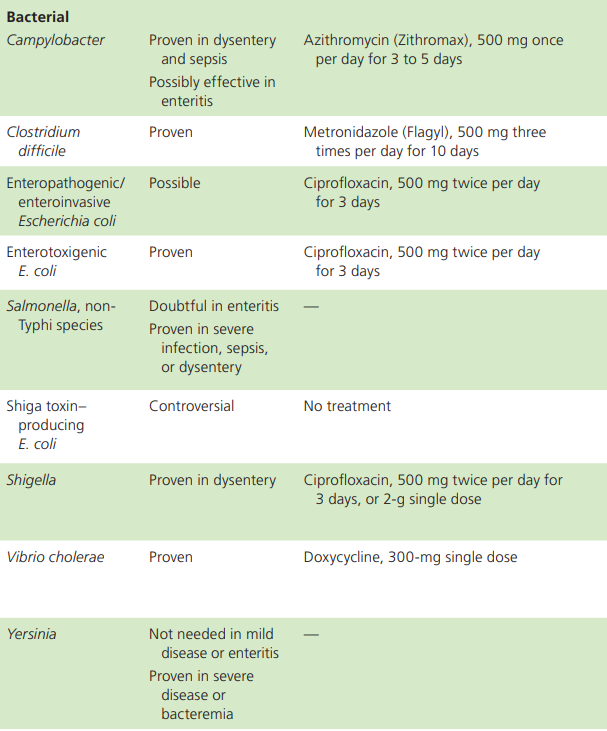
ANTIBIOTIC THERAPY
overuse of antibiotics can lead to resistance (e.g., Campylobacter), harmful eradication of normal flora, prolongation of illness (e.g., superinfection with C. difficile), prolongation of carrier state (e.g., delayed excretion of Salmonella), induction of Shiga toxins (e.g., from Shiga toxin–producing E. coli), and increased cost.
when used appropriately, antibiotics are effective for shigellosis, campylobacteriosis, C. difficile, traveler's diarrhea, and protozoal infections.
Antibiotic treatment of traveler's diarrhea (usually a quinolone) is associated with decreased severity of illness and a two-or three-day reduction in duration of illness. If the patient's clinical presentation suggests the possibility of Shiga toxin–producing E. coli (e.g., bloody diarrhea, history of eating seed sprouts or rare ground beef, proximity to an outbreak), antibiotic use should be avoided because it may increase the risk of hemolytic uremic syndrome. Conservative management without antibiotic treatment is less successful for diarrhea lasting more than 10 to 14 days, and testing and treatment for protozoal infections should be considered. Antibiotics may be considered in patients who are older than 65 years, immunocompromised, severely ill, or septic.
PROBIOTICS
ZINC SUPPLEMENTATION
'Learning > Medicine' 카테고리의 다른 글
| Nongenital Herpes Simplex Virus (0) | 2021.08.21 |
|---|---|
| Corticosteroid injection for adhesive capsulitis in primary care: a systematic review of randomised clinical trials (0) | 2021.08.20 |
| ISOLATED HYPERBILIRUBINEMIA (0) | 2021.08.18 |
| ELEVATED ALKALINE PHOSPHATASE (0) | 2021.08.18 |
| 아이폰, 아이패드에서 쓸만한 의학 어플 정리 (0) | 2011.06.14 |


